Rob Beatty, MD FACEP
Otitis Externa with Ear pain is a common complaint in healthcare. If you work in family practice, urgent care, or the emergency department, you will see patients with ear pain. Otitis media is a frequent diagnosis in patients with ear pain, especially during cold and flu season.
Otitis externa is another common diagnosis for ear pain but is typically seen more during the warmer months. This review helps to understand the pathophysiology, risk factors, symptoms, and treatment of otitis externa.
Background
Otitis externa is also known as swimmer’s ear. Otitis externa occurs when there is a breakdown of the skin-cerumen barrier in the external ear canal. Cerumen acts as a defense mechanism for the ear canal by promoting an acidic environment that inhibits bacterial growth.
The cerumen-skin breakdown then results in inflammation and edema of the ear canal. This then leads to obstruction and pruritis, causing the patients to scratch the ear canal. The scratching causes alterations in the cerumen in the ear canal, creating an alkaline environment.
The moist, dark, and warm alkaline environment is now the ideal condition for bacterial growth.
The most common pathogens that cause otitis externa are Pseudomonas aeruginosa (41%) and Staphylococcus aureus (15%). Fungal infections can also cause Otitis externa but are a low percentage of cases (2-10%) and usually only occur in patients who are immunocompromised.
Risk Factors for Otitis Externa
There are several risk factors for otitis externa. The most common risk factor, and the one patients are most familiar with, is swimming (which is where the name “swimmer’s ear” comes from). Trauma to the ear canal (e.g., excessive cleaning or scratching the ear canal) that can result in small breaks in the skin is also a risk factor.
Additionally, objects that occlude the ear (e.g., hearing aids, earbuds, diving caps) can increase the risk for otitis externa. Specifically, earbuds are becoming a more common cause of otitis externa with more people opting for in-ear headphones than traditional over-the-ear headphones. Dermatologic conditions can also predispose patients to otitis externa, such as atopic dermatitis, allergic contact dermatitis, and psoriasis.
This reference slide was taken from our Clinical Toolkit – CLICK TO LEARN MORE
Symptoms
The most common symptoms of otitis externa are pain and discharge from the ear. Pruritis tends to be the first symptom, but most patients are not bothered enough by this symptom alone to seek care. Pain is a common symptom and most of the patients I have seen with otitis externa have been in more pain than those patients with otitis media. The discharge is typically white or yellow and many people describe it as a crusting at the entrance of the ear canal. patients may also have fever, sensation of fullness in the ear, and difficulty hearing. While a fever can be present, a patient with otitis externa who has both fever and malaise should be referred to ENT or ED for further evaluation, as this can signal the disease process extends beyond the ear canal.
Exam Findings
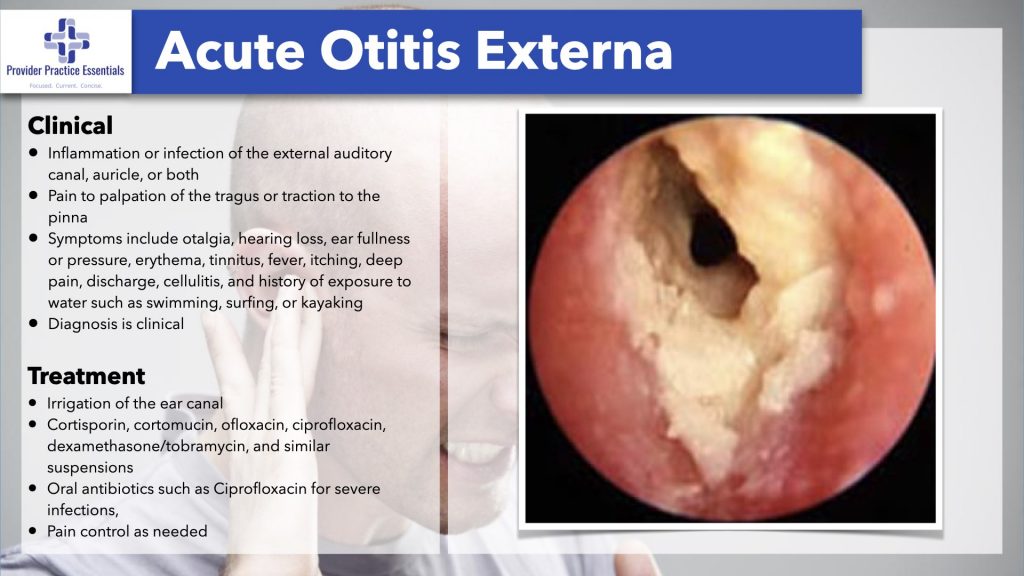
On physical exam, most patients are extremely sensitive when you initially try to position the ear to use the otoscope. Patients will have tenderness of the auricle and tragus. The ear canal can be difficult to look at due to the amount of discharge in the canal. Gentle suction can be used to remove the discharge if the patient can tolerate it. This may be necessary to visualize the tympanic membrane. Visualization of the TM is important to rule out otitis media with a ruptured tympanic membrane.
The ear canal itself is usually edematous and can be erythematous. Visualization of the other ear canal is recommended to determine what the normal canal looks like as some people can have narrow ear canals that resemble edema as their normal state. The ear canal will also appear different if there is a fungal infection present and can have a dark coating or white, sebaceous discharge.
It can be difficult on the exam to determine if there is an underlying otitis media. It is not common that otitis externa and otitis media would occur at the same time. The tympanic membrane can be erythematous in both otitis media and otitis externa. The key differentiating factor is the air-fluid level on the tympanic membrane is indicative of otitis media and not otitis externa.
Malignant Otitis Externa
One important differential diagnosis to rule out with otitis externa is malignant otitis externa. Malignant otitis externa occurs when the infection spreads to the bone surrounding the ear and is typically associated with patients who are immunocompromised, older, or have diabetes. The classic finding is granulation tissue on the ear canal floor and necrosis may also be present. If a patient has pain out of proportion to the clinical exam, malignant otitis externa should be considered and additional testing with CT or MRI should be ordered.
Treatment of Otitis Externa
Treatment of otitis externa starts with cleaning out the ear canal. This should be done as part of the exam but is also necessary in the treatment of otitis externa to ensure that any otic preparations prescribed can treat the infection. The recommended method is through either direct visualization and ear curette or if the tympanic membrane is intact, gentle irrigation.
Treatment can be divided into if the tympanic membrane is known to be intact or if the status of the tympanic membrane is unknown or not intact.
The first group of patients would be those with mild disease (i.e., minor discomfort, pruritus, edema) and intact tympanic membrane that would be treated with acetic acid-hydrocortisone. In patients with moderate disease (i.e., intermediate pain and pruritis with partially occluded canal) with intact tympanic membrane the recommended treatment is an antibiotic and glucocorticoid preparation. The recommended first-line agents are ciprofloxacin dexamethasone or neomycin-polymyxin B-hydrocortisone.
If the status of the tympanic membrane is unclear or not intact, then neomycin-polymyxin B hydrocortisone and acidic agents should be avoided. In patients with severe disease (i.e., intense pain, completely occluded canal, regional lymphadenopathy, fever, auricular or periauricular cellulitis) and intact tympanic membrane the recommended treatment is the same as moderate disease, with additional consideration for possible wick placement, IV antibiotics, and culture of the drainage.
Treatment Pearls
I have learned several pearls in practice over the years. The first is the consideration of cost when treating patients with otitis externa. Neomycin-polymyxin B-hydrocortisone is the most affordable treatment option if antibiotics are needed with it costing about $20-40 on average. Ciprofloxacin- dexamethasone can be expensive if patients do not have insurance with the cost being $60-80. Another option is to use ophthalmic ciprofloxacin in place of otic ciprofloxacin. Ophthalmic ciprofloxacin is 0.3% concentration vs. the otic solution is 0.2%. This does not include a steroid so oral prednisone or dexamethasone could be used to help the pain.
An important part of patient education is also the avoidance of water in the ear for 7-10 days. Swimming should be avoided during that time and when bathing a co4on ball coated with petroleum can be used in the ear canal to prevent water from getting into the canal. Ear plugs can be used when swimming in the future to decrease the risk of getting otitis externa. There has not been definitive evidence that using an alcohol or vinegar solution ager swimming is beneficial in preventing infection.
Otitis externa is being seen more often in clinics across the United States due to the increased use of earbuds in all age groups. This diagnosis is easily visualized on an otoscopic exam and requires a different treatment than otitis media. Prompt recognition and treatment help to relieve patient pain and increase patient satisfaction.
References:
Goguen LA. External otitis: pathogenesis, clinical features and diagnosis. Post TW, ed. UpToDate. UpToDate Inc. Accessed October 13. https://www.uptodate.com/contents/external-otitis-pathogenesis-clinical-features-and-diagnosis
Goguen LA, Durand ML. External otitis: treatment. Post TW, ed. UpToDate. UpToDate Inc. Accessed October 13, 2023. https://www.uptodate.com/contents/external-otitis-treatment
