Lindee Abe, APRN
Appendicitis is an immediate concern when any patient presents with right lower quadrant abdominal pain. The first diagnosis that comes to mind for most clinicians, and even most patients, is appendicitis. Appendicitis can happen at any age and requires surgical intervention…or does it? There have been changes in the past several years for options available for imaging and treatment.
Clinical Suspicion
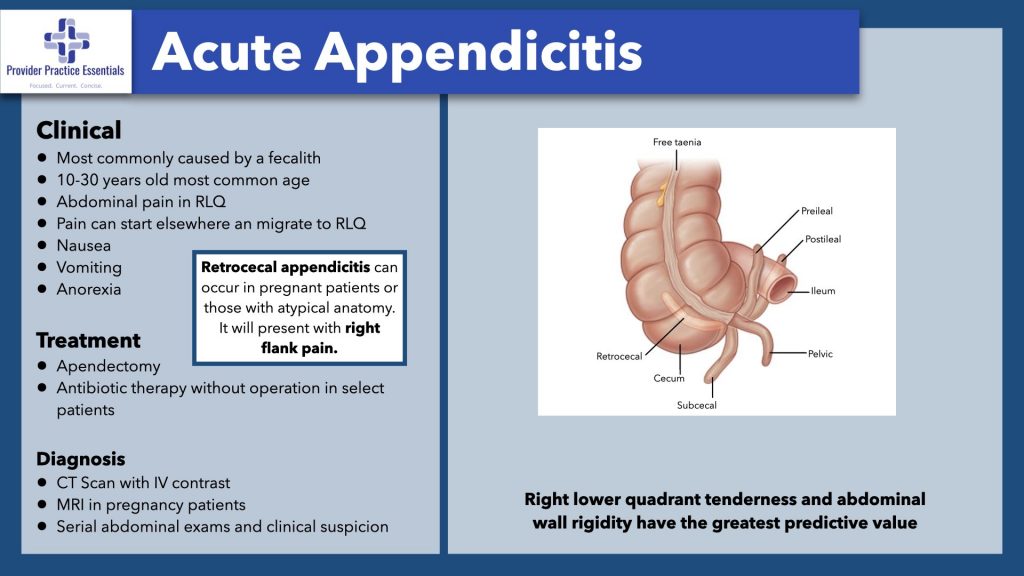
Prior to diagnosing and treating, clinicians must know when to suspect appendicitis. Appendicitis occurs when there is inflammation of the appendix, which is in the right lower quadrant of the abdomen. This inflammation can be the result of stool being lodged in the appendix (fecalith), viral infection, parasites, or bacterial infection. Normally, our appendix is not necessary in our day-to-day life, and we are unaware it is there until there is inflammation. If this inflammatory response progresses, it can lead to a ruptured (complicated) appendicitis causing all the bacteria in the intestines to spill into the peritoneal cavity. This is then a a surgical emergency. An abscess of the appendix is another possible diagnosis and requires surgical intervention.
Physical Exam Findings
Right lower quadrant pain is the hallmark symptoms of appendicitis, but that isn’t the only place patients can report pain. Some patients have pain that is located around the umbilicus. Approximately 30% of patients have a retroperitoneal retrocecal appendix1. The retroperitoneal retrocecal appendix will cause pain in the right flank area, leading the clinician to other diagnoses like nephrolithiasis.
This reference slide is taken from our Professional Development Packages – CLICK TO LEARN MORE
Another exception is in the pregnant patient. A pregnant patient, especially one that is farther along in her pregnancy, will have the appendix displaced upwards. The typical test question on boards involves a patient with nausea and vomiting with pain in the periumbilical area that travels to the right lower quadrant. This can happen in practice, but every patient will present differently. In fact, that presentation only occurs in approximately 50% of patients with appendicitis.
Other signs and Symptoms
There are other signs and symptoms that can be indicative of appendicitis. Unfortunately, none of the additional signs and symptoms by themselves apply exclusively to appendicitis.
Nausea is seen in 90% of patients
Vomiting in 75% or patients.1 Anorexia is seen in almost all patients. Low grade fever is another sign, but patients can also be afebrile. Guarding is also a symptom of peritonitis resulting from a ruptured appendix. There are two calculators available to help determine the level of concern for appendicitis:
| Alvarado | PAS | ||||
| Predictor | Detail | Value | Detail | Value | |
| symptoms | migration | 1 | 1 | ||
| anorexia | 1 | 1 | |||
| nausea-vomiting | 1 | 1 | |||
| signs | tenderness right lower quadrant | 2 | 2 | ||
| rebound pain | rebound | 1 | cough/ percussion/ hopping | 2 | |
| fever | ≥37.3 ○C | 1 | ≥38.0 ○C | 1 | |
| laboratory | leukocytosis | ≥10,000/mm3 | 2 | ≥10,000/mm3 | 1 |
| neutrophilia | ≥75% | 1 | ≥7500/mm3 | 1 | |
| total | 10 | 10 | |||
Signs of Peritoneal Irritation
There are several specific physical exam tests for peritoneal irritation with ruptured appendicitis.
- Psoas sign is pain with extension of the right leg, which is specific for a retroperitoneal retrocecal appendicitis.
- The obturator sign is pain with internal rotation of the right leg specific for a pelvic appendix.
- Rovsing’s sign is positive if there is pain in the right lower quadrant when pressure is applied to the left lower quadrant.
- Dunphy’s sign is pain with coughing.
These are all helpful tests, but if they are negative they do not rule out appendicitis. There is also the problem of children answering “yes” and reporting they have pain to every test even if they don’t have pain. One trick that learned in practice is to have the pediatric patient jump up and down or jump up to give a high five. If they do this without pain, it is unlikely that there is peritoneal irritation. However, if they refuse to do it or have pain with jumping, it will indicate there is potentially some peritoneal irritation.
Workup
There are numerous tests that can be performed during a workup for abdominal pain:
Complete Blood Count
A CBC is standard for adnominal pain and 80% of patients with appendicitis will have an elevated white blood cell count.1 The CBC will also show neutrophilia in 95% of patients. However, these can also be elevated in numerous other abdominal pathologies. Interestingly, elderly patients having an elevated band count has a high-predictive value for appendicitis.
C-Reactive Protein
The C- reactive protein, or CRP is another lab that measures inflammation. This can also be elevated in appendicitis but has a poor predictive value. However, it is noted that when looking at a patient that has all three, an elevated white blood cell count, neutrophilia, and elevated CRP, it is more predictive for appendicitis.
Imaging
In almost all patients with abdominal pain, imaging is needed at some point. It used to be that a CT abdomen/pelvis with oral contrast was the test of choice for abdominal pain. Luckily, medicine has changed, and we no longer need to wait for the oral contrast to take effect to get answers. Appendicitis can be seen on x-ray, but its absence does not rule out appendicitis.
Ultrasound
Ultrasound is now a frequently ordered diagnostic test to rule out suspected appendicitis, especially in pediatric patients. If inflammation is present in the appendix, it will measure greater than 6mm on ultrasound.
CT Scanning
CT scan does have advantages over ultrasound, specifically that it can better identify a normal appendix. There are two types of CT scans available: CT scan abdomen/pelvis and appendiceal scan with rectal contrast2. The appendiceal scan will provide better diagnostic results, but the CT scan abdomen/pelvis can also identify other underlying causes of abdominal pain.
Magnetic Resonance Imaging
MRI is another option that will be used in pregnant patients with suspected appendicitis. If chosen, it should be noted that the scan time may be delayed due to staffing or machine availability. Also, image quality may not be as reliable as ST imaging. The American College of Obstetrics and Gynecology (ACOG) considers both CT and MRI to be preferred studies.
Treatment of Appendicitis
There are now more treatment options available to patients with appendicitis. If their appendix is ruptured or there is an abscess of the appendix, then surgery will be needed. However, if the patient does not have signs of peritoneal irritation, nonsurgical management may be an option.
Nonsurgical Management
Other contraindications to nonsurgical treatment advanced age and appendicoliths. This means some patients can be treated with oral antibiotics in an outpatient setting. Outpatient antibiotic regimens for appendicitis include fluoroquinolones with metronidazole or a third-generation cephalosporin with metronidazole, or amoxicillin3. There is a catch with nonoperative management of appendicitis. Initially, approximately 90% of patients treated with nonoperative management will not have to undergo an appendectomy3. However, anywhere from 15%-49% will have a recurrent episode of appendicitis, typically between 4-7 months later. In fact, during the first year after treatment with antibiotics, it has been shown that only 30% go on to require an appendectomy.
This newer approach of not immediately resorting to surgical treatment for cases of appendicitis without complications or risk factors for progression has caused much debate among clinicians. The new current recommendations highlight a perfect scenario to utilize shared decision making with the patient. Patients that are adults and can’t afford to take time off for surgery or have more risks associated with surgery may find management with antibiotics the superior choice. However, there may be other patients that don’t want to risk the possibility of recurrent appendicitis that leads to more ED visits and may eventually have a surgical outcome. This is discussion that is best to be had between the patient and the surgeon.
Summary
Appendicitis is a well-known condition to the public and clinicians alike. There have been some shifts in the diagnostic imaging and management of appendicitis in the recent years that clinicians should be aware of in order to provide optimal care to their patients. Appendicitis is a disease process that will continue to present itself to emergency rooms and clinics and we need to be prepared to have discussions with these patients regarding treatment options.
References:
- D. Mike Hardin, J. (1999, November 1). Acute appendicitis: Review and update. American Family Physician. Retrieved March 6, 2023, from https://www.aafp.org/pubs/afp/issues/1999/1101/p2027.html#:~:text=Most%20of%20th %20time%2C%20the,peritoneum%20when%20it%20is%20inflamed.
- Pender, N. (2006, March 1). CT scans in the diagnosis of appendicitis. Journal of Ethics | American Medical Association. Retrieved March 6, 2023, from https://journalofethics.ama-assn.org/article/ct-scans-diagnosis-appendicitis/2006- 03#:~:text=When%20using%20CT%20to%20diagnose,or%20other%20signs%20of%2in flammation.
- UpToDate. (n.d.). Retrieved March 6, 2023, from https://www.uptodate.com/contents/management-of-acute-appendicitis-in-adults
