Types of Shock and Therapeutic Interventions
Do you know the four types of shock and how to manage shock patients based on they type of shock they are in? If shock patients are not routine in your practice, this review will re-familiarize you with them and the therapeutic interventions recommended for treatment.
What are the four types of shock?
Shock is defined as inadequate perfusion to the tissues, leading to an imbalance between oxygen delivery and demand. This imbalance state leads to poor tissue oxygen delivery and a transition from aerobic to anaerobic metabolism. Lactate is produced, leading to anion gap metabolic acidosis.
The four types of shock are: hypovolemic, distributive, cardiogenic, and obstructive.
While all types of shock can lead to multi-organ failure, it is critical to differentiate which shock state your patient is suffering from because the therapeutics are different. It is possible that the patient may suffer from a combination of shock types, which will complicate management.
Let’s examine the types of shock using a few case scenarios.
Shock Case Scenario #1:
A 56 year old female with no known PHMx was brought to your urgent care by a family member because she had not been eating or drinking for the past week as she had been feeling depressed by the loss of her job. The patient is awake and alert, but reports feeling lethargic and weak. Her VS are: HR 125, RR 27, BP: 83/45, SpO2: 95% on RA, Temp: 99F Axillary. Sodium 124, K 2.7, Cl 89. All other labs non-significant.
- What shock state is she in? Hypovolemic shock.
- What is the treatment?
- Large bore IV access and fluid resuscitation with balanced crystalloid such as LR, Normosol, or Plasmalyte (NS is also fine if not given in large quantities)
- Oral hydration if possible
- Electrolyte repletion.
- Repeat labs after electrolyte repletion. Given that she is at an urgent care, a transfer to a higher level of care is necessary due to due frequent reassessment of BP and electrolytes.
Shock Case Scenario #2:
A 90 year old male with PMHx of COPD, CAD, and CKD was brought to your ED from a nursing facility due to decreased mental status. On presentation, he is alert but confused. His VS are: T 103F, HR 115, BP 83/45, SpO2 93% on 6lpm NC. Labs and CXR are pending. The nursing staff noticed foul smelling urine when they were attempting to place an indwelling urinary catheter.
- What shock state is he in? Distributive shock (septic shock), likely urinary source, but will also need to assess blood and urine cultures in addition to obtaining a CXR.
- What is the treatment? Fluid resuscitation, antipyretics, broad spectrum antibiotic plus gram positive coverage (he resides in a nursing facility), and vasoactive support with norepinephrine
- What are the resuscitation goals? Mean arterial pressure is the most common objective measurement in that organ perfusion typically decreases as MAP decreases. The surviving sepsis campaign guidelines (2016) suggest a MAP of >65mmHg as achieving higher MAP goals was not associated with improvement in mortality (SEPSISPAM trial, 2014). However, for those with chronic hypertension, higher MAP targets were associated with decreased in risk of renal dysfunction.
Shock Case Scenario # 3:
A 43 year old male presents to the ED obtunded. His friends said that he was at the bar and was consuming large amount of shots over a short amount of time. Per reports, he suddenly lost consciousness and fell. He was emergently intubated and placed on the ventilator. While it was reported that he had vomited prior to intubation, his ventilator settings are unremarkable and his VS are stable. You had just placed a right IJ central line and went to call the ICU for a transfer. The RN calls you and reports that his BP is now 60/40. His is tachycardiac and looks pale.
You noted that his neck veins are distended and he has no breath sounds on the right chest. His trachea is also deviated away from the right chest.
- What shock state is he in? Obstructive shock (tension pneumothorax as the etiology).
- What is the treatment? Needle decompression, followed by CXR and definitive chest tube. He may need to have vasoactive support with norepinephrine.
Shock Case Scenario #4:
An 80 year old male was brought to the ED after he becoming more somnolent and weak for the past couple of days. His family is on vacation but he is being cared for by a neighbor. The neighbor does not know the patient’s PMHx but brought you his medication list that includes: carvedilol, sacubitril-valsartan, spironolactone, bumetanide, potassium supplements, sildenafil, and various herbal agents. His HR is 60, BP 75/43, T 99, RR29. There is cardiomegaly and bat wing pattern in the lung fields. You note that there is some type of implanted cardiac device in his left upper chest. NT-proBNP is pending.
- What shock state is he in? Cardiogenic shock, based on his medication list and CXR.
- What is the treatment? A combination of an inotropic agent such as dobutamine (or epinephrine) and norepinephrine to help improve systolic function and vasoactive support. Obtain an EKG and a TTE (formal or bedside) to assess cardiac function.
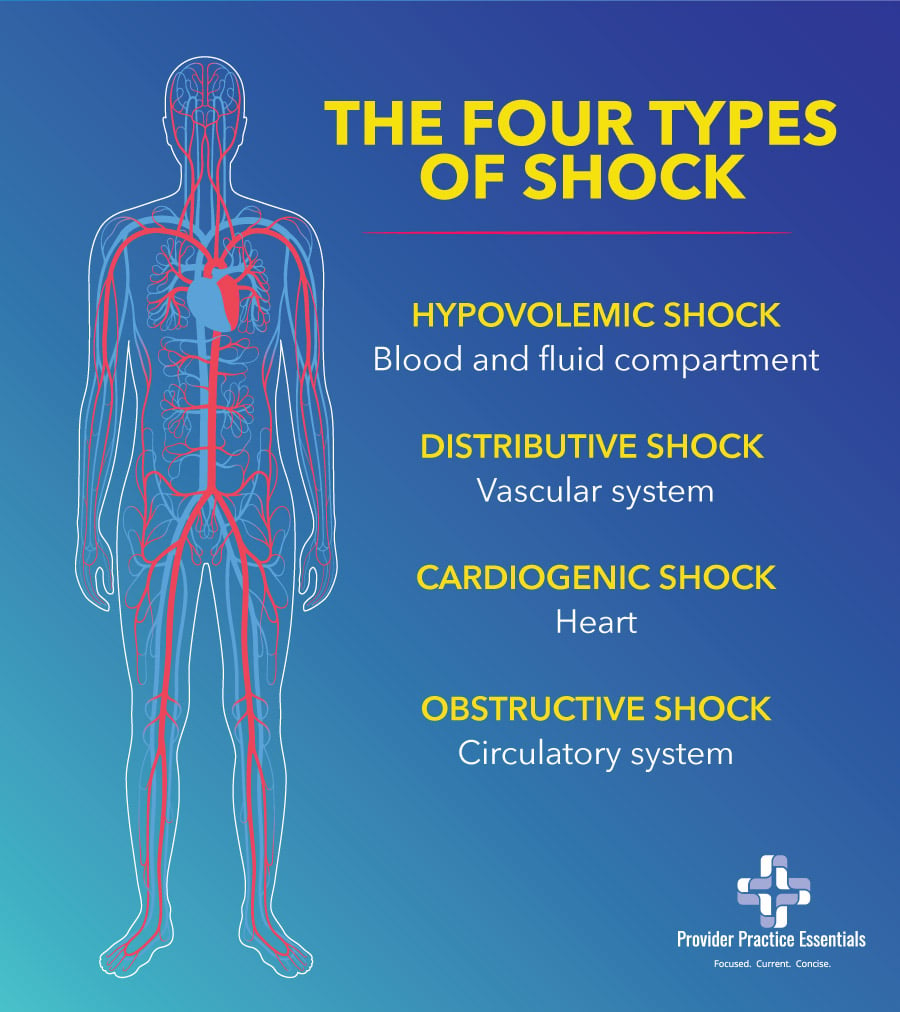
Types of Shock and Organ Systems
In the above clinical scenarios presenting the different types of shock, you can see that the common feature is the severe mismatch between the supply and demand of oxygen. The four types of shock can be assigned to a derangement in four organ systems:
- Hypovolemic shock – blood and fluid compartment
- Distributive shock – vascular system
- Cardiogenic shock – heart
- Obstructive shock – circulatory system
Hypovolemic shock
Hypovolemic shock is caused by loss of intravascular volume and is usually acute. Some of the causes may be due to acute blood loss (trauma, GI bleeding), diarrhea, inadequate fluid intake, or excessive vomiting.
Distributive shock (DS)
Distributive shock (DS) is a state of relative hypovolemia due to pathological redistribution of intravascular volume. DS includes septic shock, anaphylactic shock, and neurogenic shock. It is the most common form of shock.
Septic shock (SS)
Septic shock (SS) is a dysregulated response by the body to an infection resulting in life-threatening organ dysfunction/damage. A patient is in SS state if the lactate level is >2mmol/L and persistent hypotension requiring the administration of a vasoactive agent(s) to keep the MAP > 65mmHg, and there is suspicion of an infection.
Cardiogenic shock
Cardiogenic shock is caused by a critical reduction of the heart’s pumping capacity, leading to impaired ventricular filling and reduced ejection fraction.
Obstructive shock
Obstructive shock can be classified according to the location of the obstruction in the circulatory system in relation to the heart. Common causes of obstructive shock are pulmonary embolism, cardiac tamponade, tension pneumothorax, and high PEEP. Other causes may be due to mediastinal tumor or aortoiliac occlusive diseases.
It is important to accurately and promptly diagnose obstructive shock and its cause, as the patient can rapidly decompensate. In the PEA algorithm, the 4H’s” and “4T’s” rule of reversible causes of cardiopulmonary failure involves three obstructive shock causes: pulmonary embolism, cardiac tamponade, and tension pneumothorax.
Vasoactive and Inotropic Treatments for Shock
The treatment goal for shock is to restore tissue perfusion and is based on the etiology of the shock such as the administration of blood and blood products in hypovolemic shock secondary to trauma.
In the case of anaphylaxis, a form of distributive shock, the treatment is IM epinephrine, along with IV corticosteroids, H1 and H2 antagonist, and fluids. However, in most shock states the utilization of vasoactive and/or inotropic agents are required to support hemodynamic targets.
Thus, that leads to the question:
What is the difference between vasoactive and inotropic agents?
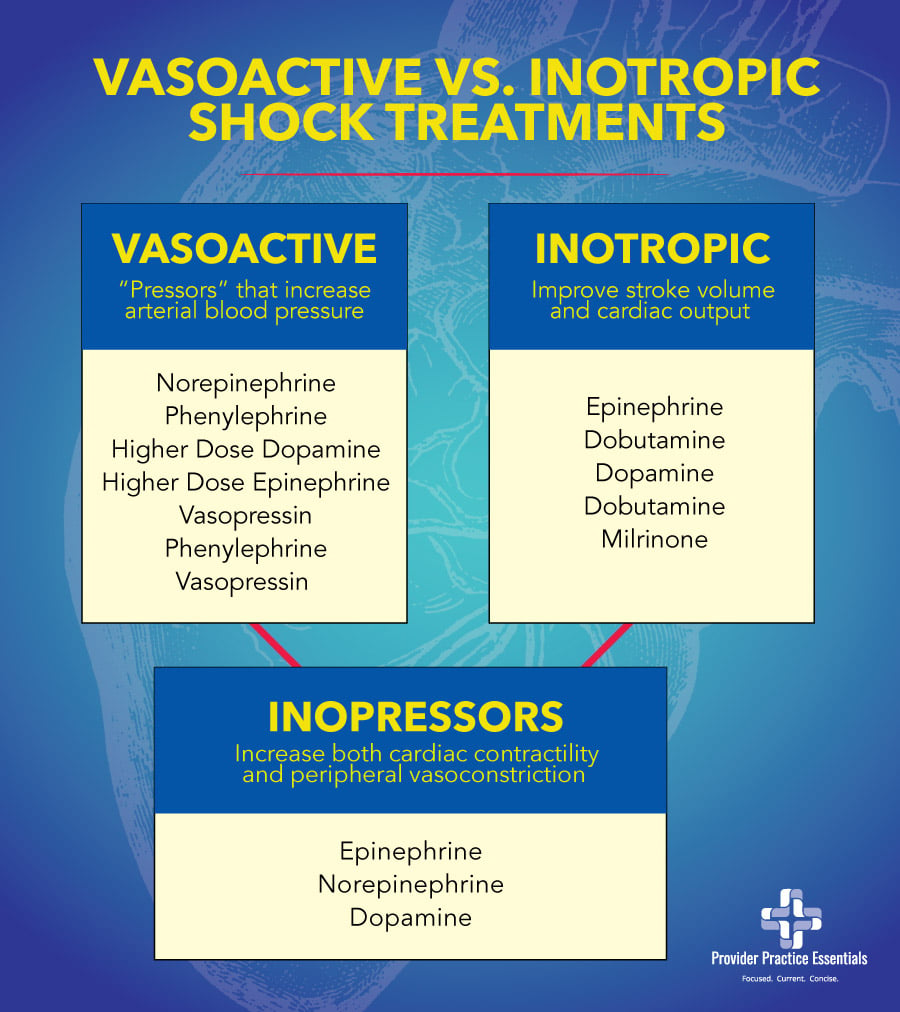
Vasoactive agents
Vasoactive agents, also known as “pressors” will increase the afterload by vasoconstriction and thereby increasing arterial blood pressure. This depends on the specific pressor, dose, and receptors involved. Examples of pressors include norepinephrine, phenylephrine, higher dose dopamine, higher dose epinephrine, and vasopressin. Phenylephrine and vasopressin are known as pure pressors and can cause a drop in cardiac output for patients in cardiogenic shock or those with heart failure with profoundly reduced ejection fraction.
Inotropic agents
Inotropic agents increase cardiac pump function or contractility, thereby improving stroke volume and cardiac output (CO = HR x SV). Examples of inotropic agents include: epinephrine, dobutamine, dopamine, and milrinone (not utilized in the ED setting). Dobutamine is an inotropic agent that may decrease vasomotor tone and blood pressure.
However, some of these agents are known as inopressors in that they both increase cardiac contractility and peripheral vasoconstriction. These agents include epinephrine, norepinephrine, dopamine. In general, vasopressors are the preferred choice for hypotension due to distributive or obstructive shock. For patients in cardiogenic shock, an inopressor such as norepinephrine, epinephrine, and dopamine may be considered.
It is important to note that norepinephrine is the first line agent in distributive shock that is refractory to fluid administration as well as in obstructive and hypovolemic shock. Vasopressin can also be added if the target MAP is not achieved. In low output cardiogenic shock, dobutamine may be initiated in combination with norepinephrine. If there is clinical evidence of volume overload (see clinical scenario #4), vasopressor and/or inotropes may be initiated earlier, in addition to IV diuretic.
While vasoactive and or inotropic agents are the mainstay therapy in shock, it only temporizes the situation. The cause of the shock needs to be established so that appropriate intervention can be provided.
References:
ASC/ASE Medical student core curriculum. (n.d.) American College of Surgeons Division of Education. Retrieved from https://www.facs.org/-/media/files/education/core-curriculum/shock.ashx
Brubaker, S. (2018). AN evidence approach to pressors in shock: part I. Retrieved from http://www.emdocs.net/evidence-based-approach-pressors-shock-part/
Squara, P., Hollenberg, S., & Payen, D. (2019). Reconsidering Vasopressors for Cardiogenic Shock. Chest, 156(2), 392 – 401
Standl, T., Annecke, T., Cascorbi, I., Heller, A. R., Sabashnikov, A., & Teske, W. (2018). The Nomenclature, Definition and Distinction of Types of Shock. Deutsches Arzteblatt international, 115(45), 757–768. https://doi.org/10.3238/arztebl.2018.0757 Vasopressor and inotropes usage in shock. (2019). Retrieved from http://www.surgicalcriticalcare.net/Guidelines/Vasopressors%20and%20Inotropes%20in%20Shock%202019.pdf
Did you find this article helpful? Check out our Clinical Skills and Procedure Workshop!





























