Introduction
Congestive heart failure (CHF) is a chronic condition characterized by the heart’s inability to pump blood efficiently, leading to fluid accumulation and finally pulmonary congestion. ECG (electrocardiogram) is a valuable diagnostic tool used in the evaluation of patients with CHF and can also provide important insights into the underlying cardiac abnormalities. This brief article aims to discuss the ECG changes commonly observed in patients with CHF and also pulmonary edema, based on current medical knowledge.
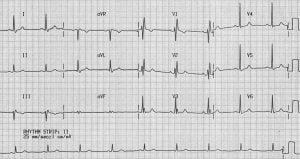
ECG Changes in Congestive Heart Failure and Pulmonary Edema:
Left Ventricular Hypertrophy (LVH):
Voltage criteria for LVH, such as increased R-wave amplitude in leads V5 and V6, and increased S-wave depth in leads V1 and V2.
Increased duration of the QRS complex (> 0.12 seconds) may indicate LVH.
Atrial Fibrillation (AF):
Irregularly irregular rhythm with absent P waves and fibrillatory waves.
Rapid ventricular response due to irregular conduction of atrial impulses to the ventricles.
Bundle Branch Blocks:
Left bundle branch block (LBBB) characterized by a widened QRS duration (> 0.12 seconds) with broad and notched R waves in leads I, aVL, V5, and V6, and also deep S waves in leads V1-V3.
Right bundle branch block (RBBB) characterized by a widened QRS duration with broad and slurred S waves in leads I, V5, and V6, and also broad R waves in leads V1-V3.
ST-Segment and T-Wave Abnormalities:
ST-segment depression and T-wave inversion may be present, reflecting myocardial ischemia or strain due to left ventricular dysfunction.
Flattening or inversion of T waves may also occur in multiple leads.
QRS Axis Deviation:
Left axis deviation may be present due to left ventricular enlargement.
Right axis deviation can occur in the presence of right ventricular hypertrophy or also dilation.
Low Voltage:
Reduced amplitude of the QRS complexes (< 5 mm in limb leads and < 10 mm in precordial leads) may be observed due to fluid accumulation in the chest.
Conclusion
ECG changes observed in patients with congestive heart failure and pulmonary edema provide valuable diagnostic information regarding underlying cardiac abnormalities. The presence of left ventricular hypertrophy, atrial fibrillation, bundle branch blocks, ST-segment and T-wave abnormalities, QRS axis deviation, and low voltage can be indicative of heart failure and its associated complications. Understanding and recognizing these ECG findings can aid in the diagnosis, risk stratification, and management of patients with congestive heart failure and pulmonary edema.
References
Liao J, Khalid N, Chodosh EH, et al. Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. GUSTO-1 (Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries) Investigators. N Engl J Med. 1996 Jan 18;334(3):481-7.
Surawicz B, Childers R, Deal BJ, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol. 2009 Mar 17;53(11):976-81.
Wang K, Asinger RW, Marriott HJ. ST-segment elevation in conditions other than acute myocardial infarction. N Engl J Med. 2003 Feb 13;349(7):2128-35.
Birnbaum Y, Sclarovsky S, Mager A, et al. ST segment depression in pulmonary embolism. J Am Coll Cardiol. 1997 May;29(6):1210-3.
Surawicz B. Electrocardiographic changes in congestive heart failure. Cardiol Clin. 1998 Aug;16(3):413-34.
Maisel AS, Krishnaswamy P, Nowak RM, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002 Jul 18;347(3):161-7.
Pulignano G, Del Sindaco D, Tavazzi L, et al. Clinical features and outcomes of elderly outpatients with heart failure followed up in hospital cardiology units: Data from a large nationwide cardiology database (IN-CHF Registry). Am Heart J. 2002 Jun;143(6):45-55.